As discussed in The Homoeopathic Heritage, Dr. Sinchan Das proposes that Alzheimer’s may originate as much in our patterns of thinking and suppressed emotions as in the brain’s neural circuits.
A Silent Global Crisis
Alzheimer’s disease (AD), the most common form of dementia, affects over 55 million people worldwide. Traditionally, it has been viewed as a neurodegenerative brain disorder characterized by amyloid plaques, tau tangles, and progressive neuronal death. Yet despite decades of research, anti-amyloid drugs have yielded only marginal benefits. This discrepancy has led researchers like Dr. Sinchan Das to look beyond the conventional neuropathological paradigm.
In his recent paper published in The Homoeopathic Heritage, Dr. Das challenges the notion of Alzheimer’s as a purely cerebral disease. He argues that the roots of AD may lie within a triad of interconnected systems — cognition, emotion, and immunity. His integrative theory synthesizes evidence from neuroscience, psychoneuroimmunology, and homeopathic philosophy, presenting a radically holistic interpretation of neurodegeneration.
From Brain Lesions to Broken Patterns of Thinking
According to Dr. Das, Alzheimer’s may begin with subtle distortions in thinking patterns — particularly alexithymic tendencies, where individuals struggle to identify or express feelings and rely excessively on logic or external details.
“Cognitive rigidity and chronic emotional suppression,” writes Dr. Das, “limit the brain’s adaptive flexibility, preventing neuroplastic repair mechanisms from functioning effectively.”
Recent studies support this: people with Alzheimer’s exhibit altered activity in the default mode network — a brain system tied to self-reflection, emotional recall, and empathy. Dysfunction here can mirror long-standing patterns of detachment or unprocessed inner conflict.
The Hidden Cost of Suppressed Emotion
Emotionally, Dr. Das highlights the role of suppression — especially of anger, grief, or guilt — in predisposing individuals to chronic stress and neuroinflammatory states. When emotions are habitually repressed, the hypothalamic–pituitary–adrenal (HPA) axis stays activated, flooding the body with cortisol and pro-inflammatory cytokines.
Over time, this constant “background inflammation” may breach the blood–brain barrier and harm neurons. Functional imaging studies reveal that emotionally avoidant individuals show reduced limbic activation and impaired hippocampal regulation — the very regions first affected in Alzheimer’s.
“Emotional repression,” Dr. Das explains, “acts like an unexpressed fever — invisible, yet systemically damaging.”
The Autoimmune Turn
In parallel, growing biomedical evidence reframes Alzheimer’s as an autoimmune-like disorder. Rather than being a toxic by-product, amyloid-β might be part of the brain’s innate immune defense — produced to neutralize pathogens or toxins. However, under sustained stress or molecular mimicry, this defense can turn self-destructive.
Dr. Das connects this to his homeopathic framework: “The same force that protects the organism, when misdirected by unresolved psychic tension, may begin attacking its own structure.”
In this model, the immune system becomes the mirror of the suppressed mind. The body’s attempt to silence inner conflict manifests as an overzealous immunological reaction, leading to chronic neuroinflammation and cognitive decline.
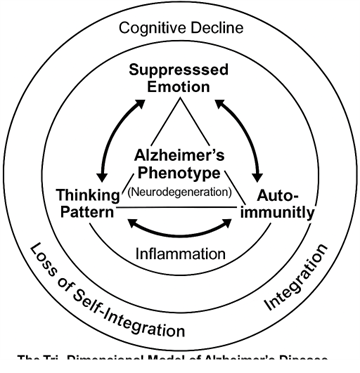
Dr. Das’s Tri-Dimensional Model: Mind, Emotion & Immunity
Dr. Das proposes a Tri-Dimensional Integrative Model, illustrated conceptually as an interlocking triangle:
1. Cognitive Style — Habitual thinking patterns (rigid logic, low introspection, alexithymia).
2. Emotional Regulation — Chronic suppression, unresolved trauma, emotional detachment.
3. Immune Integrity — Dysregulated inflammation, autoimmune tendencies, blood–brain barrier disruption.
Each domain influences the others dynamically. For instance, cognitive rigidity limits emotional processing; suppressed emotion perpetuates immune stress; immune imbalance feeds back into neural dysfunction — forming a self-amplifying loop that culminates in neurodegeneration.
Critique & Future Directions
Skeptics note that emotional and immune abnormalities may be symptoms rather than causes of Alzheimer’s. Yet, Dr. Das’s model invites a broader conversation: if chronic emotional dysregulation and autoimmune misfires precede pathology, early psychological and immunological screening could revolutionize prevention.
Further research, he suggests, should explore:
- Biomarkers linking emotional suppression with immune activation.
- Interventional studies combining psychodynamic therapy with immune-modulating treatments.
- Comparative outcomes in patients treated under integrative vs. conventional frameworks.
A Shift Toward Holistic Neuroscience
By viewing Alzheimer’s not just as a disease of the brain but as a breakdown of mind–body harmony, Dr. Sinchan Das bridges medical science and humanistic medicine. His framework re-humanizes dementia research, emphasizing the role of inner life, emotional health, and systemic balance.
“Perhaps,” he concludes, “the cure for Alzheimer’s lies not in eradicating plaques but in restoring coherence — between how we think, what we feel, and how our body defends us.”